Abstract

Introduction: Health disparities for underrepresented U.S. minority populations with hematologic cancers contribute to differential treatment and higher death rates. The Hispanic population (including people of Mexican, South/Central American, Cuban, Puerto Rican, or other Spanish-speaking cultures, regardless of race) collectively constitutes the largest minority group in the United States. Hispanic patients have been reported to have an increased incidence of B-cell acute lymphoblastic lymphoma (B-ALL) and acute promyelocytic leukemia (APL). While APL is associated with favorable outcomes compared to other acute leukemias, registry data suggest poorer outcomes in Hispanic patients with both acute lymphocytic leukemia (ALL) and acute myeloid leukemia (AML). The Hispanic paradox is an epidemiological paradox that refers to the finding that Hispanic patients have paradoxically comparable, or better, health outcomes compared to their U.S. non-Hispanic White counterparts despite barriers to care such as lower socioeconomic status. This paradox has also been reported in hematologic malignancies. Definitive data regarding differences in outcome between Hispanic and non-Hispanic patients with acute leukemias (AL) are lacking.
We sought to compare outcomes of Hispanic patients and non- Hispanic patients with acute leukemia with access to care, and examine whether the Hispanic paradox reported in hematologic malignancies is attributable to enrichment of patients with highly curable disease such as APL.
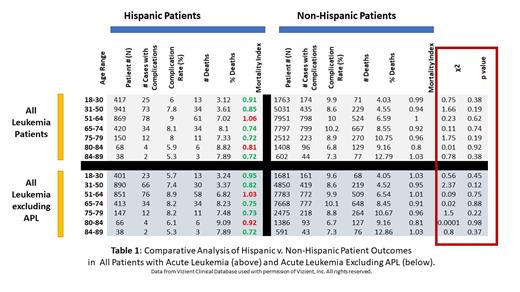
Methods: Using data from a Vizient Clinical Data Base, a healthcare claims database, we identified patients with leukemia using ICD 10 codes for acute leukemia. Adult patients with AL, ages 18-89 who were treated between January 2020 and June 2021 were evaluated. Data from 121 academic centers was included. We focused on academic centers to limit the impact of access to care . Demographic information was obtained from the registry, to which ethnicity was self-reported. Patients were stratified by age, and we compared complication rates, number of complications, number of deaths, percent deaths and mortality index between Hispanic and non-Hispanic patients. The key metric used to compare outcomes of Hispanic patients with non-Hispanic patients was the severity adjusted mortality index, which is the ratio of observed mortality over expected mortality for patients with the same diagnosis in this registry. Chi-squared test is used for to determine the statistical significance of differences in mortality (by age group) in Hispanics v. non-Hispanic patients. Initial analysis included all patients with acute leukemias, and the data was subsequently reanalyzed excluding patients with APL, as APL is known to portend a favorable prognosis.
Results: A total of 29,967 patients were with acute leukemia were evaluated; of these patients, 2903 identified as Hispanic and 27,064 were non- Hispanic. As seen in table 1, patients of Hispanic origin generally had lower treatment related complication rates in all age groups compared to their age matched non-Hispanic counterparts. Except for the 51-64 and 80-84 age groups the mortality index was lower in Hispanic patients compared to non-Hispanic peers. Differences in mortality between Hispanic and non-Hispanic patients in all age groups were not statistically significant. Trends to a lower mortality index in Hispanic patients are highlighted in green in table 1. When patients with APL were excluded from the analysis, the trend lower mortality in Hispanic patients in most age groups persisted. Again, the mortality index was comparatively higher in hispanic patients in the 51-64 and 80-84 age groups, but differences in mortality between Hispanic and non- Hispanic patients were not statistically significant. Exclusion of APL patients did not have a significant impact on the complication rate or mortality supporting that the Hispanic paradox is independent of higher rates of very favorable risk myeloid malignacies in this population.
Conclusions: Hispanic patients with access to academic cancer centers have the potential for non-inferior outcomes compared to non-Hispanic patients. Equivalent outcomes as assessed by mortality index were not attributable solely to the higher incidence of very favorable risk disease such as APL in the Hispanic population.
Watts: Takeda: Consultancy, Research Funding; Genentech: Consultancy; Rafael Pharma: Consultancy; Celgene/BMS: Consultancy. Bradley: Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees; AbbVie: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Sekeres: Takeda/Millenium: Membership on an entity's Board of Directors or advisory committees; BMS: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal